Arthrogenic Muscle Inhibition (AMI)
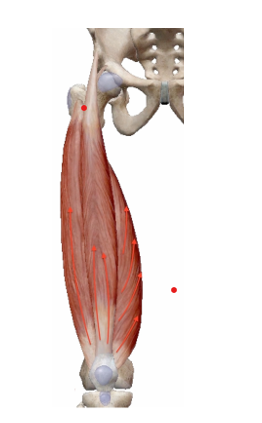
Persistent weakness in the quadriceps muscles and limited knee extension following knee injuries/surgeries stem from distinct changes in neural excitability; a phenomenon referred to as arthrogenic muscle inhibition (AMI).
Comprehension of the pathophysiology underlying AMI is essential to the physical therapist as it serves as a compass for therapeutic interventions.
Several factors contribute to the onset of AMI including pain, edema, effusion, receptor damage, and joint laxity. Arthrogenic muscle inhibition occurs when signals from a joint provide feedback via the spinal cord to alert the brain there is damage to the area. The typical neurological response is to inhibit muscles around that joint, reducing pressure and mitigating further damage. While the quadriceps muscles themselves are not damaged, there is an inability to recruit motor units of the muscles surrounding the involved joint. Initially protective, this reflex can lead to muscle atrophy and subsequent weakness, hampering functional recovery over time. Proper treatment and interventions to restore quadriceps function is crucial to a full neuromuscular recovery for a safe return to activity and reduce the risk of reinjury and osteoarthritis.
Initial AMI
AMI up to 6 weeks post-operative is typically a spinal reflex inhibition.
Long-Term AMI
AMI present greater than 6 months post-operative leads to neuroplastic changes and cortical reorganization.
Presentation of AMI
After a knee injury or surgery, Acute Muscular Inhibition (AMI) can manifest in different forms, such as:
- Vastus Medialis Obliquus (VMO) muscle weakness,
- Hamstring contracture leading to limited knee extension
- Persistent extension limitations
- Atrophy of the quadriceps
Risk Factors for AMI:
- Immobilization
- Swelling
- Prolonged use of crutches
- Pillow support under the knee
- Pain
- Multiple ligament injury
The Bottom Line
- AMI is a change in the pattern of neural muscle recruitment of muscles around the involved joint.
- AMI is a protective mechanism in the acute phase post-injury and post-operatively (4-6 weeks)
- AMI perpetuated beyond the acute phase leads to supraspinal neuroplastic changes.
- Chronic AMI can contribute to hamstring contractures, limiting functional knee extension.
- Quick resolution of AMI beyond the acute phase is crucial to positive outcomes and to help prevent reinjury.
Keep tuned to our future blogs for discussion on treatment approaches for AMI.